- Al Hafid N, Christodoulou J (October 2015). "Phenylketonuria: a review of current and future treatments". Translational Pediatrics. 4 (4): 304–17.
- "Press Announcements - FDA approves a new treatment for PKU, a rare and serious genetic disease". www.fda.gov.
- "National Institutes of Health Consensus Development Conference Statement Phenylketonuria: Screening and Management". NICHD. October 16–18, 2000.
- Bernstein LE, Rohr F, Helm JR (2015). Nutrition Management of Inherited Metabolic Diseases: Lessons from Metabolic University. Springer. p. 91. ISBN 9783319146218.
- Cannon Homaei S, Barone H, Kleppe R, Betari N, Reif A, Haavik J (November 2021). "ADHD symptoms in neurometabolic diseases: Underlying mechanisms and clinical implications". Neuroscience and Biobehavioral Reviews. 132: 838–856.
- Marcdante K, Kliegman RM (2014). Nelson Essentials of Pediatrics (7 ed.). Elsevier Health Sciences. p. 150.
- Kalter H (2010). Teratology in the Twentieth Century Plus Ten. Springer Science & Business Media. pp. 89–92. ISBN 9789048188208.
- Camp KM, Parisi MA, Acosta PB, Berry GT, Bilder DA, Blau N, et al. (June 2014). "Phenylketonuria Scientific Review Conference: state of the science and future research needs". Molecular Genetics and Metabolism. 112 (2): 87–122.
- "Phenylketonuria (PKU) Test". HealthLink BC.
- Berry SA, Brown C, Grant M, Greene CL, Jurecki E, Koch J, et al. (August 2013). "Newborn screening 50 years later: access issues faced by adults with PKU". Genetics in Medicine. 15 (8): 591–9.
- "Phenylketonuria (PKU)". Madriella Doula Network. Madriella Network. 14 October 2016. Retrieved 11 April 2021.
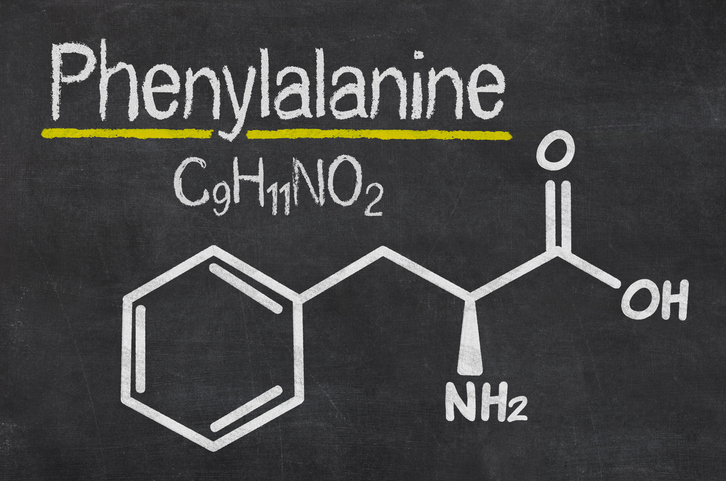
- "Phenylketonuria". MarkerDB. Wishart Research Group.
- Burton BK, Jones KB, Cederbaum S, Rohr F, Waisbren S, Irwin DE; et al. (2018). "Prevalence of comorbid conditions among adult patients diagnosed with phenylketonuria". Mol Genet Metab. 125 (3): 228–234
Phenylketonuria: What is it and how is it manifested? (hyperphenylalanemia)
Photo source: Getty images
Most common symptoms
Show more symptoms ᐯ
Phenylketonuria and its treatment: Medications and diet
Show more