- Joos E, Bourgeois P, Famaey JP (June 1993). "Lymphatic disorders in rheumatoid arthritis". Seminars in Arthritis and Rheumatism. Elsevier BV. 22 (6): 392–398.
- Grada AA, Phillips TJ (December 2017). "Lymphedema: Diagnostic workup and management". Journal of the American Academy of Dermatology. 77 (6): 995–1006.
- Sleigh BC, Manna B (January 2020). "Lymphedema". StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing.
- Grada AA, Phillips TJ (December 2017). "Lymphedema: Pathophysiology and clinical manifestations". Journal of the American Academy of Dermatology. 77 (6): 1009–1020.
- Martin MB, Kon ND, Kawamoto EH, Myers RT, Sterchi JM (October 1984). "Postmastectomy angiosarcoma". The American Surgeon. 50 (10): 541–545.
- Chopra S, Ors F, Bergin D (December 2007). "MRI of angiosarcoma associated with chronic lymphoedema: Stewart Treves syndrome". The British Journal of Radiology. 80 (960)
- Requena L, Sangueza OP (February 1998). "Cutaneous vascular proliferations. Part III. Malignant neoplasms, other cutaneous neoplasms with significant vascular component, and disorders erroneously considered as vascular neoplasms". Journal of the American Academy of Dermatology. 38 (2 Pt 1): 143–75, quiz 176–8.
- Publishing, Licorn (2009-10-28). "Body image and quality of life in secondary lymphedema of the upper limb". Servier - Phlebolymphology.
- "Oncology Fact Sheet" (PDF). aota.org. Retrieved 2019-09-03.
- "A Visual Guide to Lymphedema". WebMD.
- Shenoy, R. K. (2008-09-20). "Clinical and Pathological Aspects of Filarial Lymphedema and Its Management". The Korean Journal of Parasitology. 46 (3): 119–125.
- "Lymphoedema - Causes". nhs.uk. 2017-10-20.
- Jeannie Burt; Gwen White (1 January 2005). Lymphedema: A Breast Cancer Patient's Guide to Prevention and Healing. Hunter House. pp. 9. ISBN 978-0-89793-458-9.
- Choices, NHS. "IPS retired". nhs.uk.
- Brorson H, Ohlin K, Olsson G, Svensson B, Svensson H (June 2008). "Controlled compression and liposuction treatment for lower extremity lymphedema". Lymphology. 41 (2): 52–63.
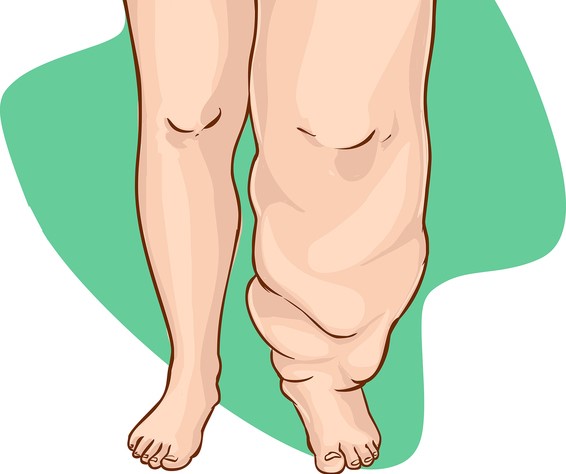
Lymphedema: What is it and how does it manifest? + Treatment

Photo source: Getty images
Most common symptoms
Show more symptoms ᐯ
Lymphedema and its treatment: lifestyle interventions and medications
Show moreLymphedema is treated by
Other names
lymphoedema